Pregnancy is both a magical and confusing time. There are so many changes going on in a pregnant woman’s body to prepare for the new life growing inside of her. Exercise is often a point of question and concern for pregnant women. Pregnant women are often told that they should not exercise during pregnancy, however, recent research has been demonstrating the benefits of exercise in modulating pregnancy side effects, as well as eased pain during labor, delivery, and even postpartum recovery. There are many individual factors that play a role in determining if a person is appropriate for a certain type of exercise, which should always be discussed with your healthcare provider first.

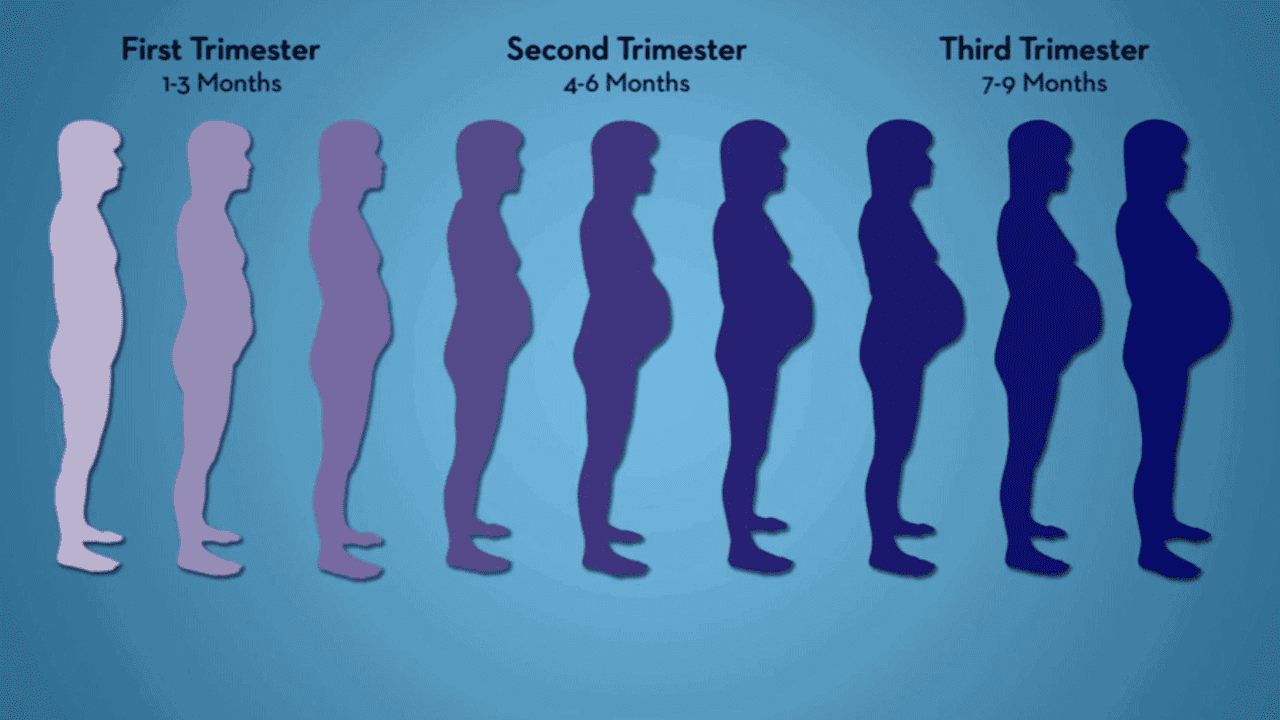
The general guideline presently is to continue the type of exercise your body was used to before pregnancy, and modify the appropriate way to keep you and baby safe. This means that if you were already doing yoga, it is considered safe to continue this activity. In the same sense, if your pre-pregnancy body was used to weight lifting, it is considered safe to continue this activity with certain modifications. Common modifications for general exercise will be discussed later in this blog, but always talk to your health care provider/obstetrician prior to starting/continuing exercise during your pregnancy. There are different recommendations for exercise during each trimester of pregnancy, based on how you and baby are both changing and developing.
Disclaimer: Discuss with OB/PCP before starting a new exercise program or with any specific
concerns about your individual experience.
First Trimester
Challenges
The first trimester of pregnancy is one where you are normally not feeling your best. You may be overwhelmed at the news of your pregnancy, with lingering questions nagging at you until your first prenatal appointment. You may be struggling to work out and figure out what you are allowed/not allowed to do. During this time, many women experience morning sickness (that sometimes is not just limited to the morning), making it harder to work out. Many women also experience a decrease in energy levels as the baby rapidly grows and develops inside your womb. At this point, the placenta is not fully developed, and therefore the hormonal, nutritional, and energy demand is heavier on you.
Benefits of Exercise
Exercise during this time can actually be extremely beneficial in preventing recurrence of morning sickness. By getting your heart rate up, your body can accommodate to the noxious stimulus associated with morning sickness, and reduce its occurrence. Exercise can also help boost mood, improve sleep quality, reduce bloating, and set the base for muscle tone and strength needed later in pregnancy.
Modifications
During this time, your main modifications are going to be based on how your body feels and reacts to exercise. Keeping your heart rate in a training level that is below maximal ranges can be more tolerable compared to high intensity exercise at this time. A quick and easy way to figure out where you should be training is to use this equation:
220 – your age = max heart rate
Once you have determined your max, you can multiply this by a certain percentage (I used between 60-80% as an appropriate tolerance during my first trimester) to determine your target heart rate range during exercise. *Your healthcare provider and/or physical therapist can help you to find your individual, optimal range.*
For me, I am 27 years old, so my max heart rate is 193 bpm. My target heart rate training range was between 60-80% of my max. This meant that I aimed to keep my heart rate between 115-154 bpm during training on average. This is just an example based on my experience, symptoms, and tolerance to exercise at the time to prevent from overexerting myself.
Normal resting heart rate can be anywhere from 60-100 bpm, but this can vary person to person based on pre pregnancy fitness level, medical conditions, and medications taken. To determine an appropriate training level for you, discuss your medical history, as well as your fitness history with your healthcare provider. Your physical therapist can also be a great resource for determining an appropriate fitness program for you during your pregnancy.
Using a target heart rate range early on can help keep your body moving safely and comfortably throughout your pregnancy. When your heart rate exceeds your tolerated range, switch to an active recovery exercise to slowly bring your heart rate back down to your target range. This can be lowering your training weight/resistance, your speed of performance, or taking out a jump and switching to a step instead depending on whatever exercise form you are participating in.
Another helpful modification if you are already not completing one, is using a thorough warm-up and cool-down before and after your workout. This will allow your heart rate to make gradual changes, instead of sudden changes, which can also help prevent any unwanted nausea during or after exercise. Consider going for a walk after your workout to slowly bring your heart rate down.
You should also be adequately fueling your body before and after exercise. Sometimes pregnant women find it difficult to eat before and after exercising due to nausea. Getting the right nutrients in your body in a timely manner before and after your workout can help curb nausea, as well as cravings later in the day and later in your pregnancy. Eat a full, balanced meal about 1-2 hours before exercise, and a small carbohydrate snack about 30 minutes prior to exercise. This will prevent your blood sugar from dropping too low during exercise.
Second Trimester
Challenges
The second trimester is often an easier time for pregnant women. Now that the placenta is developed, there is a lot less work on mom’s body to fully support the baby, and this reduces a lot of the unwanted pregnancy side effects. Many women start to experience less morning sickness, and improved energy levels for this reason. Despite this, some women continue to experience fatigue for a different reason; as the baby increases in size, so does your belly, and this may disrupt your sleep. Sleep disruption is common in the second trimester from need to use the bathroom more frequently in the middle of the night, and trouble falling asleep in certain positions.
Furthermore, many women experience an increase in their appetite, as well as new cravings. Carrying a baby increases your body’s caloric demand, meaning how much energy your body needs to do its usual activities, so your eating habits may change. This may come with bloating or constipation. A growing baby means an increased need for blood flow. This can lead to swelling, nasal congestion, sensitive gums, and dizziness. Some women also experience leg cramps, which could be a side effect from dehydration or lacking typical vitamins/minerals in an ever changing diet.
Exercise benefits
Exercise can be helpful to moderate your weight gain during this time. Many women gain weight at different speeds during the second trimester, with some rapid weight gain in the beginning and slowed throughout the remainder of the second trimester, whereas other women gain weight in small increments throughout these 3 months. Exercise gets your body moving, which can also help moderate the effects of gas and constipation. Regular exercise can help maintain regular bowel movements, improve sleep quality, reduce nasal congestion, and help reduce swelling as circulation improves.
Modifications
Recommendations from the first trimester modifications hold true with some new additions.
Due to the increased pressure of the baby on internal organs and blood vessels, one major modification for pregnant women during this time is to avoid lying flat on your back for extended periods of time, especially during resistance training. Slight elevation of the torso on a ledge, BOSU, or wedge can be extremely helpful to allow women in the second trimester the ability to continue training. Secondly, at this point, it is no longer recommended to lay flat on your stomach. Any exercises that involve lying on your stomach (or prone) can be modified to a different position to work the same muscle group without placing too much pressure on mom and baby.
Many women wonder if they can still run/jump during the second trimester of pregnancy. This is a conversation to have with your healthcare provider, but again, the general consensus is that if you did it pre-pregnancy, and that you and baby feel good during pregnancy, you can continue to do this. As your bump gets larger, there will be more pressure placed on your pelvic floor muscles. These muscles support your bladder and uterus. If you start to notice incontinence with exercises, this is an indicator that your pelvic floor muscles are too weak to support that exercise, so talk to your physical therapist about alternatives to keep you moving.
We also recommend avoiding exercises that result in “coning” of your belly bump. This is when your belly starts to physically look like a cone during core exercises, and is very firm. This is a sign that your abdominal muscles are not strong enough to support you during that exercise, and can lead to a diastasis recti or abdominal separation later in pregnancy and post partum. This is not going to impact baby, but can make your recovery later harder, and therefore better to avoid if possible during your pregnancy exercise regime

All in all, the modifications made during pregnancy to exercise gradually occur as your belly starts to increase in size, and are largely based on how you and baby feel when you are moving, and recommendations from your healthcare provider.
Third Trimester
Challenges
Baby is making the most changes in size and movement during the transition from second to third trimester, and throughout the third trimester. For this reason, it is common to exercise more aches and pains, as well as a harder time generally moving and changing positions. Going hand in hand with this, sleep and insomnia become more prevalent during the third trimester – this may be a mix of your body achy, more frequent need for bathroom use in the middle of the night, hormonal changes, and maybe even your little one kicking you in the middle of the night.
This may increase fatigue levels during waking hours. Your body also produces a hormone called Relaxin to prepare your body for labor and delivery. This is meant to loosen your ligaments to open up your pelvis and allow an easier time for the baby to exit the womb. However, this hormone is not specific to target just the pelvic region, and therefore your ligaments and joints throughout your body may be more “relaxed.” This can contribute to some aches and pains, and seeking the help and advice of your physical therapist is best to find the best way to tackle these pains.

Exercise benefits
With a growing bump, it can be pretty difficult to get out of a chair or off of the floor. For me, the hardest thing was putting my socks on, which my husband was able to help me with. Yoga and other flexibility exercises can help reduce some of the discomfort with these tasks. Exercise in general is a great way to boost mood, and keep your body conditioned for the marathon that is labor and delivery. Exercise, even low impact, can be helpful to maintain circulation and minimize swelling in your hands and feet, as well. Pregnancy, especially at the end, can be uncomfortable, so it is important to keep your body moving in ways that you enjoy without overextending yourself. According to a study at the University of Montreal, physical activity during pregnancy can help boost babies’ brain functions, so if you don’t do it for yourself, do it for your brilliant baby!
Post-Partum
Now that baby is here, you need to allow your body proper time to recover from labor and delivery. Typically, there is a gradual return to pre-pregnancy activities over 6 weeks for vaginal delivery, and 8 weeks for Cesarean. Your healthcare provider, typically your Obstetrician, will have the final say in allowing you to resume activities as usual, and some activities you may be allowed to resume faster than others. Due to the wide ranges of personal recovery times based on individual birth experiences, always talk to your healthcare provider before returning to exercise of any kind, and what might be appropriate for you.
PT Interventions
Physical therapists work with pregnant women all of the time. Whether this be due to pregnancy-related aches and pains, or some other injury sustained during daily life like a non-pregnant person may get. We as therapists follow certain guidelines for your physical therapy program as stated above depending on where you are in your care.
As stated above, many women exercise neck, back, or hip pain due to the release of the hormone Relaxin during pregnancy that can weaken the ligaments in these areas. Certain exercises can be prescribed by your physical therapist in order to provide stability to these joints and reduce pain intensity/frequency. Continuing to work on deep core muscles during pregnancy, safely, can also help with labor and delivery as well as postpartum recovery.

Physical therapists can also help to address aches/pains that are persistent after your recovery period. The process of labor and delivery can be a lot for your body, and you may be left with some weaknesses in areas that you previously did not have. A physical therapist can help get you back to feeling like yourself.
No matter where you are in your pregnancy journey, be it that you just found out the positive news, or you’ve had your little one several months ago, consult with one of our Doctors of Physical Therapy to help you manage your pain and reach your goals.


